Ob-gyn faculty members come together to learn about AI, ergonomics and more
Annual professional development day offers faculty members the opportunity to enhance their careers among peers

At the ob-gyn department’s Faculty Professional Development Day (FPPD) in November, the learning ran the gamut from the very digital to the very human. Refreshingly, it all happened in person.
“It’s a pause, more or less, from the clinic. You’re here. You’re not on a Zoom meeting, where you’re distracted by something else,” said Janet Bodley, an associate professor of ob-gyn, Chief of Obstetrics and Gynaecology at Sunnybrook, and FPDD board member. “It’s invigorating.”
The main conference room at the Chestnut Residence was near capacity for the morning’s plenary session on applied artificial intelligence (AI) in health care, presented by Muhammad Mamdani, the vice-president of UHT’s Data Science and Advanced Analytics and the director of Temerty Centre for Artificial Intelligence Research and Education Medicine.
Over the years, his team has developed and employed approximately 50 AI solutions for medical practice, including one of the most popular applications, an AI scribe, which uses generative AI to automate note-taking tasks during patient consultations.
A recent Ontario study found that over three-fourths of AI scribe clinician users reported reduced cognitive load.
“About three to four hours per week were freed up for direct patient care, and over 80 per cent of participants said they’d really like to continue using it,” said Mamdani, who is also a professor in the department of laboratory medicine and pathobiology.

His team also developed CHARTWatch, an application that runs an algorithm every hour on high-risk patients, integrating 150 to 170 different parameters from their medical record to predict whether they’ll die or be transferred to the ICU in the next 48 hours. When the predicted deterioration crosses a certain threshold, CHARTWatch alerts the medical staff.
Why did they develop this early warning system? When one considers that an average clinical decision involves hundreds of parameters — and complex one thousands — it’s not a surprise we need a little help, said Mamdani.
“We collected over 300 clinician predictions, and when a physician says, ‘This patient is going to die or go to the ICU,’ they’re right less than one-third of the time.”
A trial of CHARTWatch at St. Michael’s Hospital resulted in a 26 per cent reduction in expected mortality. The study was published in the Canadian Medical Association Journal.
AI has its challenges too. For example, the algorithm is only as good as the data it’s trained on; if the data includes racial biases, then so will the outputs. Also, robust AI regulation has yet to full arrive, creating safety and privacy issues, introducing ethical quandaries, and eroding trust and reliability.

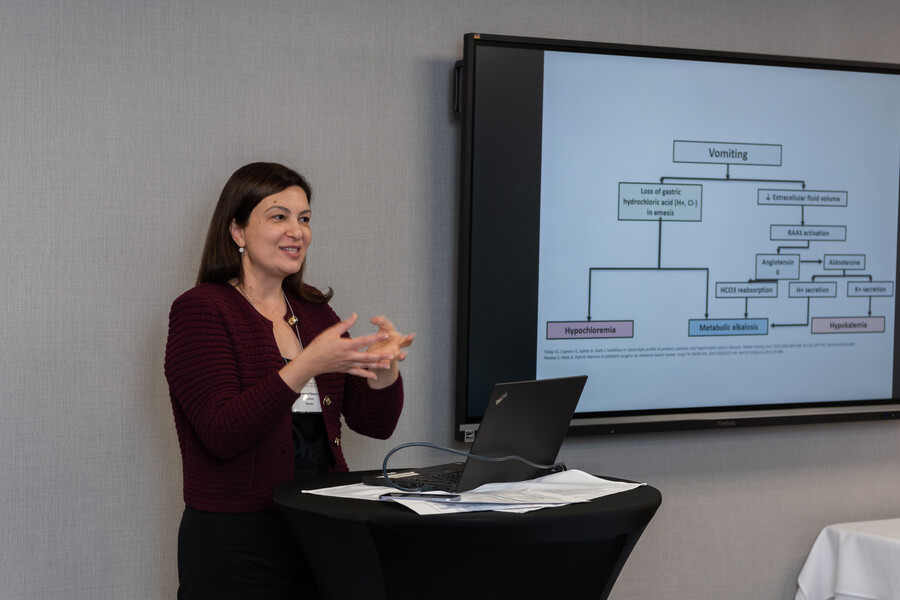
“When we talk about ergonomics in the workplace or in our environment, our equipment needs to fit. And most of the time it doesn’t,” said Olga Bougie, an ob-gyn at Sinai Health.
Bougie delivered the second plenary session on ergonomics for the ob-gyn, focusing on the physical situations — the static or high-force awkward postures particular to surgeons and practitioners — that can lead to musculoskeletal disorders (MSDs).
In a research survey she conducted, Bougie found 90 per cent of ob-gyns had pain symptoms, with laparoscopic surgery being notably injurious among surgical procedures. The neck, lower back, shoulders and right hand were cited as the body parts most affected.
Females reported more MSDs, which in part can be attributed to equipment historically developed for male stature and hand size, a mismatch that is only starting to be addressed by manufacturers.

Nearly half of surgeons, said Bougie, classify their pain as severe and take anti-inflammatories to assist them with surgery.
“If the doctor were seeing this person as a patient, a patient who’s in pain, what would they tell them? It probably wouldn’t be ‘take medication and do the next surgery’ but provide better care for yourself,” she said.
Ob-gyn work environments demand repetitive precision skills, prolonged postures, and can restrict freedom of movement. They also include many digital screens — laptops, phones and equipment displays — which can be awkward to view. There’s eye strain that accompanies that, especially when trying to extrapolate three-dimensional objects from two-dimensional images.
In addition, work shifts can sometimes run 12 to 14 hours per day, and the cognitive load demanded by the job siphons the physician’s energy to make good decisions for self-care.
What is remarkable, said Bougie, is that despite all these problems, so few reported taking time off from work.
Bougie listed some solutions, including paying more attention to three factors: the work area and equipment, your posture and movement, and your body preparation and maintenance. Resetting and changing positions at regular intervals, and 15 to 30 second movement breaks, can head off future problems. Off-hour strengthening exercises that target specific muscles can also help.
She also suggested a culture change. An atmosphere that encouraged speaking up to ask for equipment adjustments in the OR, for example, or for time off to heal, would go a long way to addressing MSDs and empower the next generation to prioritize healthy ergonomic choices.
“When we’re working in pain, it’s hard to make our best decisions and do our best work,” she said.
Small group sessions





- Physiotherapist Mitchell Starkman and Humara Edell, an assistant professor of ob-gyn and obstetrician and urogynecologist at Sunnybrook Health, taught faculty members mobility and strengthening exercises: “If you can pair a new habit with routine procedures, it’ll help,” said Starkman.
- Upton Allen, chair of the Decanal Promotions Committee and a professor of the department of paediatrics, joined Saba Khan, a manager in Temerty’s Office of Inclusion and Diversity, to talk about how equity, diversity, indigeneity, inclusion and accessibility (EDIIA) is an essential component of Temerty’s educational strategy. By providing alternate pathways to medical education for high-quality applications, EDIIA initiatives address the lack of traditional networks and supports for some candidates: “EDIIA is seen as a driver of innovation,” said Khan, also mentioning the improvement in patient care that comes with physician diversity.
- Heather Millar, a physician at Sick Kids, discussed a trauma-informed approach to patient care that shifts the conversation from “What’s wrong with you” to “What happened to you?” Trauma is about the physical and emotional reaction to an event, not the event itself, and recognizing the root of difficult behaviours in patients can lead to practical approaches to avoid further trauma, increase patient engagement and ultimately improve care.
- Susanna Talarico, an associate professor of the department of paediatrics and a paediatrician at Sick Kids, offered insights and suggestions on how to balance transformative learning with the creation of psychological safe spaces for students. Much of this centres on respectful language, beginning with teachers admitting they too are learning and may make a mistake: “Language has been used deliberately for years to oppress, to exclude, to dismiss. It can also be used to empower, to include, to uplift,” said Talarico.
Pics from the day!









Promotions to Associate Professor in 2024
- Sebastian Hobson, Full-time Clinical (MD), Mount Sinai Hospital
- Liat Hogen, Full-time Clinical (MD), Unity Health Toronto–Princess Margret Hospital
- Claire Jones, Full-time Clinical (MD), Mount Sinai Hospital
- Noor Ladhani, Full-time Clinical (MD), Sunnybrook
- Andrea Lausman, Full-time Clinical (MD), Unity Health Toronto–St. Michael's Hospital
- Colleen McDermott, Full-time Clinical (MD), Mount Sinai Hospital
- Andrea Simpson, Full-time Clinical (MD), Unity Health Toronto–St. Michael's Hospital
- Wendy Whittle, Full-time Clinical (MD), Mount Sinai Hospital
Chair's awards
| Award | Recipient |
|---|---|
| Quality Improvement and Patient Safety (QuIPS) | Amanda Cipolla |
| Postgraduate Program Development and Innovation | Michael Chaikof |
| Outstanding Research Potential | Shiri Shinar |
| Sustained Research Excellence | Ann Kinga Malinowski |
| Excellence in Research Facilitation | Sarah Ferguson |
| Excellence in Research Facilitation | Stephane Laframboise |
| Excellence in Continuing Medical Education Teaching | Rachel Kupets |
| Excellence in Continuing Medical Education Course Coordination | Lindsay Shireff |
Undergrad and postgrad awards
| Award | Recipient |
|---|---|
| Undergraduate Teaching Awards | |
| Credit Valley Hospital | Kerry Myckan |
| Mississauga Hospital | Kelly Chu |
| Mount Sinai | Mara Sobel |
| North York General Hospital | Kalpana Sharma |
| Sunnybrook | Grace Liu |
| St. Michael's Hospital | Mark Yudin |
| St. Joseph's Health Centre | Aparna Sarangapani |
| Michael Garron Hospital | Jennifer Cram |
| Etobicoke General Hospital | Wilson Chan |
| Princess Margaret Cancer Centre | Stephane Laframboise |
| Excellence in Undergraduate Teaching | Louise-Helene Gagnon |
| Excellence in Integrated Undergraduate Education | Cici Zhu |
| Master Teacher | Mara Sobel |
| Master Teacher | Jennifer Cram |
| Excellence in Postgraduate Teaching | Michelle Jacobson |
| Excellence in Integrated Postgraduate Education | Salikah Iqbal |
| John R. McArthur Scholar Award (Discretionary) | David Chitayat |
| Emeritus Contribution Award | Harold Drutz |