May 8, 2023
Ob-Gyn and LMP faculty publish paper sharing insights and successes of MHSc in Clinical Embryology
Research
Trailblazing U of T program provides template for similar programs aimed at formalizing training
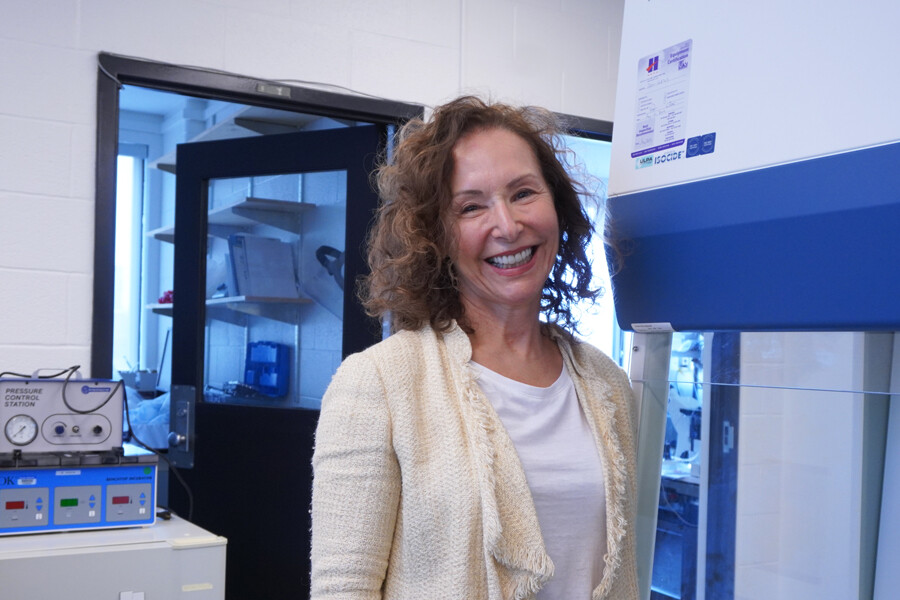
Dr. Heather Shapiro, professor of obstetrics and gynaecology, serves as program field director for the clinical embryology stream of the MHSc program in laboratory medicine.