Main Second Level Navigation
Breadcrumbs
- Home
- Education
- Global Health Opportunity: Kenya
- AMPATH-U of T Program
AMPATH-U of T Program

AMPATH-U of T partners the University of Toronto with Moi University and its teaching hospital in Eldoret to improve reproductive health in Western Kenya.
Representatives of AMPATH-U of T co-lead the Reproductive Health component of the Academic Model Providing Access to Healthcare – Reproductive Health (AMPATH-RH).
AMPATH assists the Government of Kenya in improving primary health care throughout Western Kenya. AMPATH is centered in Eldoret, the location of Moi University School of Medicine and the Moi Teaching and Referral Hospital.
The University of Toronto Department of Obstetrics & Gynaecology is the lead North American member of the Reproductive Health component of AMPATH. Indiana University School of Medicine is the lead North American institution of AMPATH.
AMPATH-U of T is improving the quality of women’s and reproductive health care in Western Kenya through a sustained partnership between Moi University School of Medicine / Moi University Teaching and Referral Hospital and the Temerty Faculty of Medicine at the University of Toronto. The partnership supports the bilateral exchange of students, residents and faculty, between Toronto and Eldoret. The exchanges, integrated across several programs, emphasize mutual benefit, professional development and education, and long-term commitment.
Our success is a result of the generous support of individuals, foundations, organizations and institutions. Your support of AMPATH-U of T is very much appreciated and we encourage you to consider donating to this worthwhile cause.
Take a look at our past stories for more information on how your donation is changing the lives of women in Western Kenya:
- Kenyan residents inspired by cutting-edge surgeries during fall elective
- Kenyan gyn-onc fellows talk about ‘eye-opening’ and ‘game-changing’ observership
- Two fellows to spend 2023 serving in Kenya
- Department hosts Kenyan residents for hands-on clinical work
- Global Women’s Health and Equity fellow partners with Access Alliance to improve reproductive care for refugees
- Moi–Toronto collaboration results in Kenya's first locally trained MFM subspecialists

Vision, goal and objectives
Vision
Academic health centres linked to all citizens have a critical role as a foundation of a sustainable health system able to address the health needs of a community.
Goal
The goal of our partnership is to improve the quality of women’s and reproductive health care in Western Kenya through the development of a sustained partnership between the Medical School of Moi University and the Faculty of Medicine of the University of Toronto focused on improving maternal and gynaecological services, continuing medical education and research.
Objectives
- Reduce maternal mortality and morbidity
- Prevent and treat gynecologic cancers
- Improve maternal and infant nutrition

Guiding Principles
- Lead with Care
- Reciprocity
- Equity
- Peer support
- Integration with the Ministry of Health

Leadership team
Dr. Kellie Murphy
Professor & Gordon C. Leitch Chair, Department of Obstetrics & Gynaecology,
Temerty Faculty of Medicine, University of Toronto
Dr. Rachel Spitzer
Vice Chair, Global Women's Health and Advocacy
Professor, Department of Obstetrics & Gynaecology
Temerty Faculty of Medicine, University of Toronto
Dr. Barry Rosen
Section Lead, Gynaecologic Oncology, Beaumont Health System
Dr. Allan Covens
Professor and Chair of the Division of Gynecologic Oncology at the University of Toronto and Sunnybrook Health Sciences Centre
Dr. Nan Okun
Head, Division of Maternal-Fetal Medicine
Associate Professor, Department of Obstetrics & Gynaecology
Temerty Faculty of Medicine, University of Toronto
Dr. Michael Milosevic
PMH Lead
Associate Director, Radiation Medicine Program, Princess Margaret Cancer Centre
Professor, Department of Radiation Oncology, University of Toronto
Joe George
Administrator, Fellowships and Global Health
Department of Obstetrics & Gynaecology
Temerty Faculty of Medicine, University of Toronto
AMPATH-RH activities
As academic health centers, the North American partners who form the AMPATH Consortium are guided by a tripartite mission that includes patient care (service), education (training), and research. While education and research are critically important to achieving our goals, AMPATH is determined to lead with care. All members of AMPATH believe beginning with service is crucial since we work with populations that are terribly underserved in health. In addition, leading with care often helps to instill a belief that the health conditions of populations can be improved. In addition, service is the foundation upon which the necessary training and research is conducted.
Research
Research is critical to improving medical care and sustaining a health system. A robust medical information system is required to provide data for research. The AMPATH medical record system (AMRS), originally conceived by the AMPATH Informatics team, is a centerpiece of AMPATH Informatics and is a cornerstone of the AMPATH initiative.
Current research projects are ongoing in the focus areas of our collaboration, such as maternal, newborn and child health, gynecologic oncology, and public health. Much of our research is programmatic, focusing on evaluating our clinical care programs to assess and improve the health outcomes for women in western Kenya. Many of our findings though are relevant in other regions of Kenya and sub-Saharan Africa.
Click here to access the most current list of research publications by AMPATH that includes U of T authors.

Education
Faculty and trainees from Moi University and the University of Toronto have the opportunity to participate in placements in reproductive health in Toronto and Eldoret, respectively. If you wish to participate, visit the Get Involved page.
Since 2005, faculty members from the University of Toronto’s Department of Obstetrics & Gynaecology have participated in placements at Moi University’s School of Medicine/Moi Teaching and Referral Hospital (MUSOM/MTRH), supporting undergraduate and faculty education. This included important core development of both Maternal-Fetal Medicine and Gynaecologic Oncology, two reproductive health subspecialties that are lacking in Kenya.

Several Kenyan Department of Reproductive Health (DRH) physicians from MUSOM/MTRH have visited the University of Toronto, conducting observerships in cervical cancer care. Each year two senior Kenyan undergraduate medical students from MUSOM completed a six-week medical rotation at Mount Sinai Hospital, St. Michael’s Hospital and Sunnybrook Health Sciences Centre in Toronto. Kenyan postgraduate OBGYN residents also conduct electives in Toronto. This allows for the development of both personal and professional relationships, a broad exposure to high-quality medical care, and a vision for Kenya’s potential.
Current objectives for educational activities
Improved maternal health
- Support the implementation MUSOM Master's of Medicine postgraduate training programme in Reproductive Health, including third-year elective placements in Toronto;
- Training and support for Community Health Workers;
- Involve medical and MPH students and residents from UofT, and MUSOM and other Kenyan universities in maternal health program;
- Continue to support maternal-fetal medicine training and fellowships.
Treatment and prevention of cervical cancer
- Provide continuing medical education and clinical support for cervical cancer screening, treatment of precancerous abnormalities and treatment of cancer with surgery and chemotherapy;
- Involve medical and MPH students and residents from UofT, MUSOM and other Kenyan universities in the oncology program;
- Continue to support gynaecologic oncology program at Moi University.
Services
Current services provided through AMPATH-UofT include:
- Advanced care in maternal-fetal medicine
- Cervical cancer screening
- Surgery to repair obstetric fistulas
- Advanced care in gynaecologic oncology
- Outreach maternity services at community level
- Mother's support groups
Every two minutes, a woman dies from complications related to pregnancy and childbirth.
Programs
AMPATH-U of T runs many programs in conjunction with the Moi University School of Medicine and the Moi Teaching and Referral Hospital, including training and teaching programs in gynaecologic oncology, maternal-fetal medicine, radiology, immunology, and others.
Maternal and child health
92%
of pregnant women attend at least one antenatal visit
43%
deliver in a health facility
44%
of births are attended by a skilled attendant
197 deaths per 100,000 live births
is the global maternal mortality rate
Kenya has made significant strides in maternal health, reducing its maternal mortality ratio from 1,375 in 2000 to 149 deaths per 100,000 live births in 2023. However, this rate remains high compared to countries like Canada, where the MMR is just 11 per 100,000.
A Kenyan woman faces a 1 in 39 lifetime risk of maternal death. Beyond mortality, many women suffer long-term health consequences, including obstetric fistula, often caused by obstructed labour. This condition not only affects physical health but also leads to emotional trauma and social ostracization.
Primary causes of maternal deaths are:
- Haemorrhage
- Sepsis
- Hypertensive disorders
- Unsafe abortions
- Obstructed labour
Barriers to safe motherhood in Kenya
The root causes of Kenya’s high maternal mortality include:
- Limited access to healthcare due to poverty and long travel distances.
- Gender inequality, where women often need permission to seek care.
- Low facility-based delivery rates: Less than half of births occur in health facilities.
- Shortage of skilled birth attendants, such as trained midwives and doctors.
Gynaecologic oncology
As of 2025, the global burden of cancer continues to rise, with projections estimating over 20 million new cases annually.
Comparing sub-Saharan Africa cancer burden to western countries
Approximately 70% of these cases occur in low- and middle-income countries, where access to prevention, diagnosis, and treatment remains limited.
In Sub-Saharan Africa, a significant proportion of cancers affecting women are gynaecologic in origin, with cervical cancer being the most prevalent. In Kenya, cervical cancer remains the leading cause of cancer-related deaths among women, with an incidence rate of 40.1 new cases per 100,000 women annually.
In contrast, in Canada, cervical cancer ranks only 11th among female cancers, and the five-year survival rate exceeds 90% due to widespread screening and early treatment.
Western countries have dramatically reduced cervical cancer mortality through organized screening programs (e.g., Pap smears and HPV testing), which detect precancerous changes early. Women with abnormal results receive timely treatment, often preventing the development of invasive cancer. Advanced cases are treated with radiation and chemotherapy, often with good outcomes.
In Kenya, however, screening coverage remains low — around 17% among reproductive-age women
Cancer affects African women in peak reproductive years
As a result, most women present with late-stage disease, which is far more difficult to treat. Although radiation and chemotherapy are standard treatments for advanced cervical cancer, Kenya has historically had only one radiation machine to serve the entire population, though efforts are underway to expand capacity.
Cervical cancer disproportionately affects women in their peak reproductive years, with devastating consequences for families and communities.
The high burden of cervical cancer in Sub-Saharan Africa is driven by limited awareness, low HPV vaccination coverage, inadequate screening, and scarce treatment infrastructure.
The gynaecologic oncology team of AMPATH-U of T, in collaboration with Moi University and other members of the AMPATH Consortium, is working to reduce disparities in gynecologic cancer care and improve outcomes for women in western Kenya.
Public health refers to all organized measures (whether public or private) to prevent disease, promote health, and prolong life among the population as a whole. Its activities aim to provide conditions in which people can be healthy and focus on entire populations, not on individual patients or diseases.
Public health
The University of Toronto's Department of Obstetrics and Gynaecology partners with the Dalla School of Public Health in working with the Moi University School of Public Health.
AMPATH took a population-based approach to developing one of the most successful anti-retroviral therapy (ART) programs in sub-Saharan Africa. Since 2009, we have been building on this success to bring primary health care to the entire population of western Kenya, 10.5 million people.
Public health expertise in biostatics, epidemiology, occupational and environmental health, social and behavioural health sciences and public health policy is helping to AMPATH support the development of a robust primary health care program throughout western Kenya.
As with all AMPATH programming, we strive to integrate care (clinical public health) with education and research.
Radiology
Our radiology team has been introducing and encouraging improved gyneacological imaging (endovaginal ultrasound approach) and teaching sterilization and disinfection techniques for a number of years now.
New and well-functional used ultrasound machines have been donated to Moi Teaching and Referral Hospital (MTRH) and rural hospitals. Training has been conducted when these donations have been made to ensure the potential benefits of the equipment are realized and the equipment is well maintained.
Current and future activities in this area include:
- Basic ultrasound instruction to medical officers
- Fetal assessment / Fetal lie
- Evaluation of amniotic fluid volume
- Placental position
- Fetal activity
- Cervix
- More sophisticated instruction for radiology residents
- Obstetrical imaging
- Gynecological imagine
- Other
- Supporting interaction between OBGYN and radiology professionals
- Taking basic ultrasound to villages

Partners
WE'RE FAR MORE IMPACTFUL TOGETHER.
AMPATH is a perfect example of what happens when people come together with a shared mission. Multiple North American academic institutions join together to make up the AMPATH Consortium, which in turn partners with the Moi University and Moi Teaching and Referral Hospital in western Kenya. Together, we exchange knowledge, share resources, train medical professionals, and expand our reach beyond patients to whole communities.
The following are the AMPATH Consortium members:
- Indiana University School of Medicine - Indianapolis, Indiana
- Brown University School of Medicine - Providence, Rhode Island
- Duke University Medical Center/Hubert-Yeargan Center for Global Health - Durham, North Carolina
- Icahn School of Medicine at Mount Sinai / Arnhold Institute for Global Health - New York, New York
- Johns Hopkins University - Baltimore, Maryland
- University of Alberta - Edmonton, Canada
- Purdue University - West Lafayette, Indiana
- University of California, San Francisco - San Francisco California
- University of Texas at Austin Dell Medical School - Austin, Texas
- University of Toronto Faculty of Medicine - Toronto, Canada
- Stanford Centre for Innovation in Global Health - Stanford, California
- NYU Langone Health - New York, New York
Partners in Toronto
In the core of Toronto exists an incredible number of organizations involved in health care. Walking up University Avenue and along College Street one passes numerous organizations involved in the Toronto Academic Health Science Network (TAHSN). This is an impressive network providing health care, conducting biomedical research, and teaching undergraduate, postgraduate, medical, and healthcare professional students. AMPATH-U of T draws on this vast expertise in health for its success.
Major Toronto-based partners include:
- Dalla Lana School of Public Health, University of Toronto
- Faculty of Medicine, University of Toronto
- Princess Margaret Cancer Centre
- Mount Sinai Hospital
- St Michael's Hospital
- Sunnybrook Health Sciences Centre
Partners in Kenya
Our partners in Kenya include:
- Moi University College of Health Sciences (MUCHS)
- Moi Teaching and Referral Hospital (MTRH)
- Government of Kenya
- Kenya Obstetrical and Gynaecological Society (KOGS)
Map of clinical sites
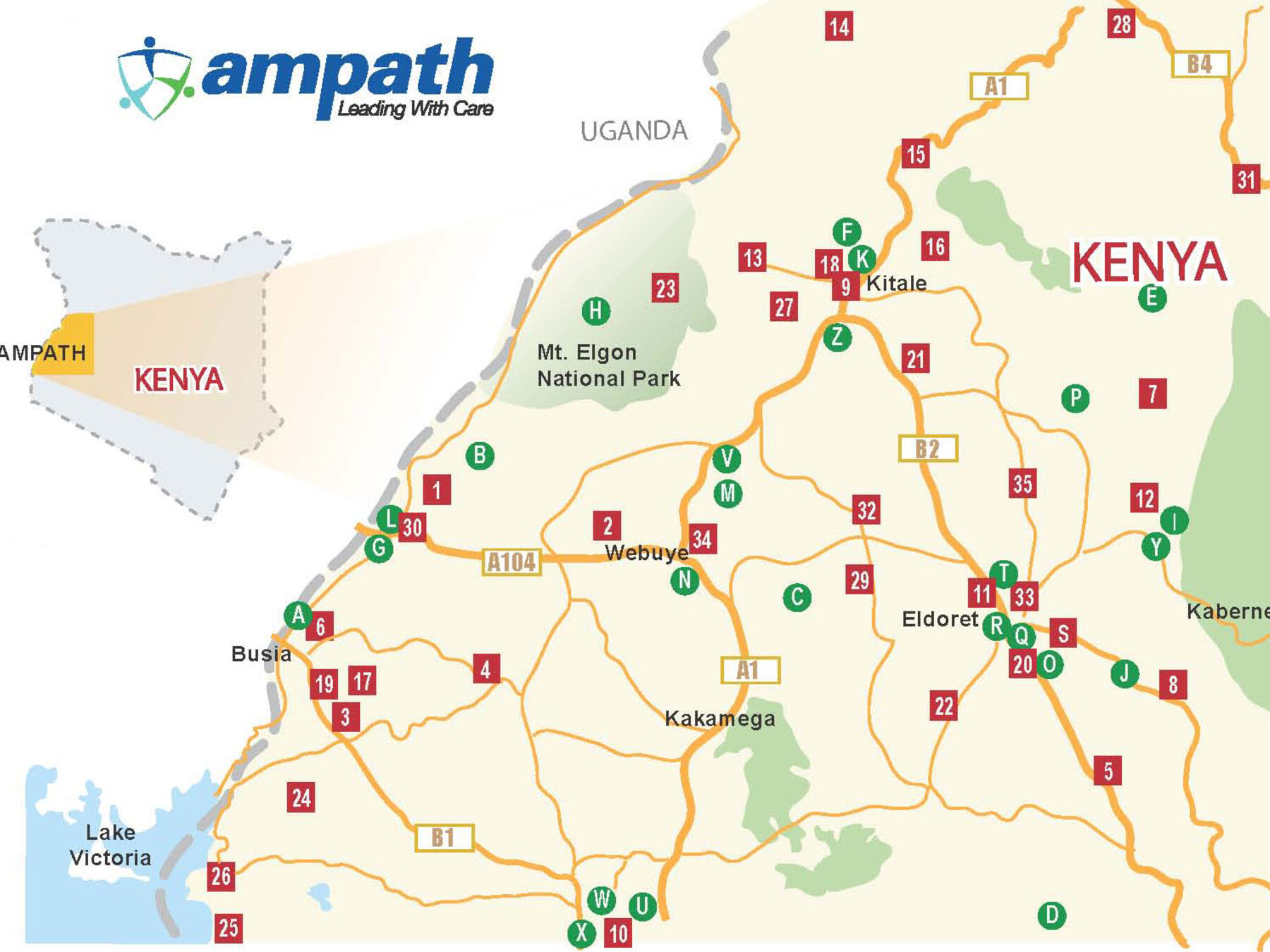
| 1 Angurai Health Centre 2 Bokolu Health Centre 3 Bumala A Health Centre 4 Bumala B Health Centre 5 Burnt Forest Sub-District Hospital 6 Busia District Hospital 7 Chebiemit District Hospital 8 Chepkorio Health Centre 9 Cherangany Health Centre 10 Chulaimbo Sub-District Hospital 11 Huruma Sub-District Hospital 12 Iten District Hospital 13 Endebess Sub-District Hospital 14 Kacheliba District Hospital 15 Kapenguria District Hospital 16 Kapsara District Hospital 17 Khunyangu Sub-District Hospital 18 Kitale District Hospital 19 Matayos Health Centre 20 Moi Teaching and Referral Hospital (modules 1-4) 21 Moi’s Bridge Health Centre 22 Mosoriot Rural Health Training Centre 23 Mt. Elgon District Hospital 24 Mukhobola Health Centre 25 Osieko Dispensary 26 Port Victoria Sub-District Hospital 27 Saboti Sub-District Hospital 28 Sigor Sub-District Hospital 29 Soy Health Centre 30 Teso District Hospital 31 Tot District Hospital 32 Turbo Health Centre 33 Uasin Gishu District Hospital 34 Webuye District Hospital 35 Ziwa Sub-District Hospital |
Satelite Clinic [Satellite to] A Busia Prison [Busia District Hospital] B Changara Calvary Dispensary [Teso] C Chepsaita Dispensary [Turbo Health Centre] D Diguna Dispensary [Mosoriot Rural Health Training Centre] E Elgeyo Border Dispensary [MTRH Modules] F GK Prison [Huruma Sub-District Hospital] G Kamolo Dispensary [Teso] H Kaptama Health Centre [Mt Elgon District Hospital] I Kapteren Health Centre [Iten District Hospital] J Kesses Health Centre [Huruma Sub-District Hospital] K Kitale Prison [Kitale District Hospital] L Malaba Health Centre [Teso] M Mihuu Dispensary [Webuye District Hospital] N Milo Dispensary [Webuye District Hospital] O Moi University Clinic [MTRH Modules] P Moiben Health Centre [MTRH Modules] Q Ngeria Prison [Huruma Sub-District Hospital] R Pioneer Health Centre [Huruma Sub-District Hospital] S Plateau Mission Hospital [Burnt Forest Health Centre] T Rai-Ply Clinic [Huruma Sub-District Hospital] U Riat Dispensary [Chulaimbo Sub-District Hospital] V Sinoko Dispensary [Webuye District Hospital] W Siriba Dispensary [Chulaimbo Sub-District Hospital] X Sunga Dispensary [Chulaimbo Sub-District Hospital] Y Tambach Sub-District Hospital [Iten District Hospital] Z Tulwet Dispensary [Kitale District Hospital |
Contact us
Medical students and residents who are interested in completing an elective with AMPATH should contact:
Dr. Rachel Spitzer
Vice Chair, Global Women's Health and Advocacy and Professor
Department of Obstetrics and Gynaecology, University of Toronto
rachel.spitzer@sinaihealth.ca
Joseph George
Administrator, Fellowships and Global Health
Department of Obstetrics and Gynaecology, University of Toronto
joseph.george@utoronto.ca